Team Creates Potentially Faster Test for Urinary Tract Infections
By: Phil Roth | May 19, 2023
Researchers at The University of Texas at Dallas have developed a prototype diagnostic sensor that might allow individuals to confirm urinary tract infections (UTIs) quickly, without having to wait 24 to 48 hours for lab test results.
Dr. Nicole De Nisco, assistant professor of biological sciences in the School of Natural Sciences and Mathematics, said the sensor could help alleviate the overuse and inappropriate use of antibiotics, which can lead to antibiotic resistance in infectious bacteria.
“If someone comes in with what they think is a UTI, some clinicians will often just give them antibiotics without waiting up to two days for lab tests to confirm that it’s a UTI,” she said. “That’s bad because there are a lot of other conditions that have similar symptoms to a UTI, but they aren’t UTIs.”
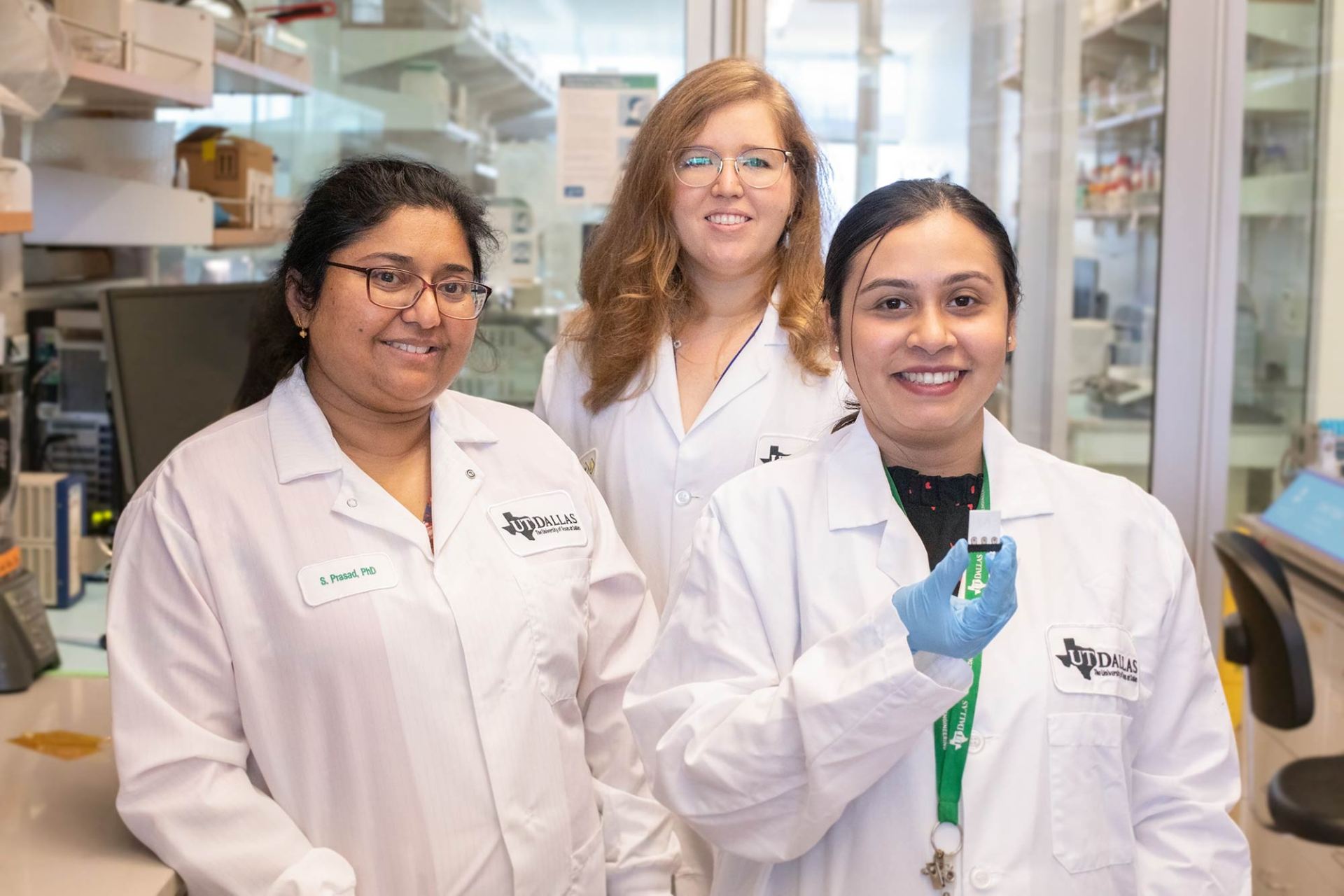
A team of researchers led by De Nisco; Dr. Shalini Prasad, department head and professor of bioengineering in the Erik Jonsson School of Engineering and Computer Science; and Dr. Philippe Zimmern, professor of urology at UT Southwestern Medical Center, is hoping to give clinicians a better tool that can more accurately diagnose UTIs within five minutes.

The new technology, which detects and determines the concentration of three protein biomarkers in urine, is currently up to 85% accurate in diagnosing a UTI.
“We’ve taken these three markers and their expression profiles, and we digitized them,” said Prasad, a Cecil H. and Ida Green Professor in Systems Biology Science and corresponding author of a recent report on the technology. “We developed a logic table that tells you what happens if the level of one molecule is low; one is high; all are low; or all are high.”
The researchers said the strategy could potentially boost the diagnostic power of current electrochemical biosensors, resulting in more precise therapy and improved patient outcomes. De Nisco said that in the future, biomarkers could potentially be swapped out so that the sensor can check concentrations of different proteins for detection of other diseases, such as kidney disease.
“We could take this technology and adapt it to any kind of urine diagnostic based on different kinds of molecules,” she said.
In addition to its use by doctors, Prasad said she envisions a sensor, much like a pregnancy test, that patients could use at home, which would be helpful for those who might be embarrassed, immunocompromised or who face cultural issues. UTIs predominantly occur in women, with 10% to 20% of U.S. women experiencing one each year.
“I come from India, where it’s culturally very challenging to go to a clinic for UTI testing; it’s something that is frowned upon,” Prasad said. “We’d like to see this device in the hands of every person who wants to use it so they can use it in the comfort of their own home.”
While there are over-the-counter UTI test strips available for home use, De Nisco said they are “incredibly inaccurate.”
“There is a big, unregulated market for UTI diagnostics and treatment, but most have not been validated by science,” she said.

To learn more about how UT Dallas is enhancing lives through transformative research, explore New Dimensions: The Campaign for UT Dallas.
The researchers are now working to improve the accuracy of their device by examining alternative biomarkers and by improving the device design to capture the flow of urine better.
Prasad said if results remain promising, clinical trials could begin in three years or so.
De Nisco said there has been little research dedicated to creating devices that accurately and quickly screen for UTIs.
“I think many of those working in the diagnostics field don’t think UTI is that big of a problem,” she said, “so it’s an area of opportunity that needs to be filled. I’m glad we have the right combination of experts who can develop a tool that could help a lot of people.”
A proof-of-concept study for the sensor was published in the March 2023 print edition of Bioengineering & Translational Medicine.
Other UTD contributors to the research included lead study author Antra Ganguly MS’17, a biomedical engineering doctoral student; and Tahmineh Ebrahimzadeh MS’21, PhD’22 and Jessica Komarovsky BS’22, former members of De Nisco’s lab.
The research was funded in part by The Welch Foundation.
Media Contact: Phil Roth, UT Dallas, 972-883-2193, phil.roth@utdallas.edu, or the Office of Media Relations, UT Dallas, (972) 883-2155, newscenter@utdallas.edu.





