Researchers Receive $4.5 Million in Funding for Cancer Projects
By: Amanda Siegfried | Oct. 1, 2018
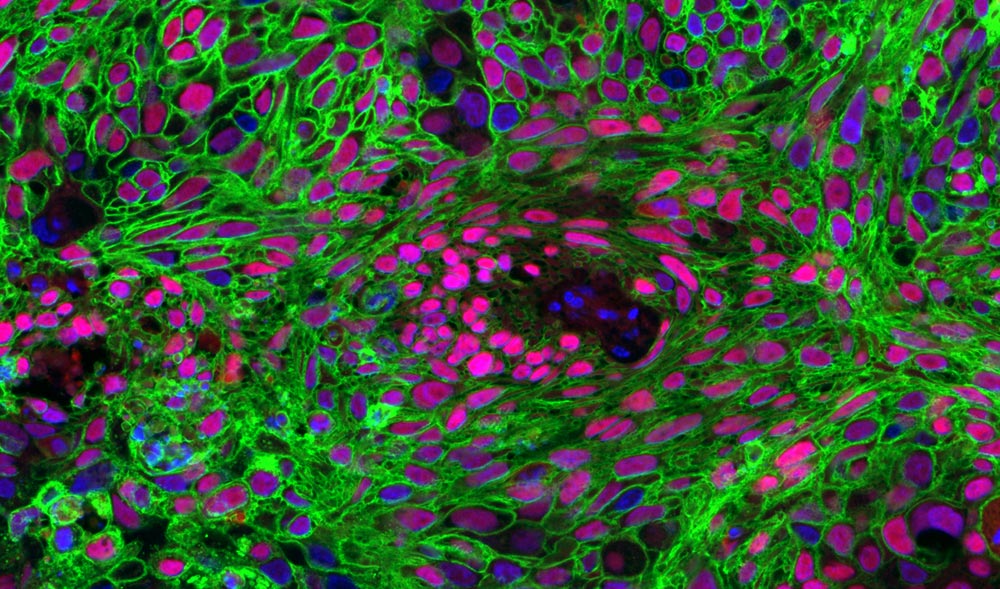
Dr. Jung-whan “Jay” Kim and his team received a grant from the Department of Defense to continue their work showing the connection of sugar to one subtype of non-small cell lung cancer. In an earlier study, they found that a glucose transporter called GLUT1 (in green) is prevalent in lung squamous cell carcinoma (above), which accounts for about 25 percent of all lung cancers.
More than $4.5 million in new funding from state and federal agencies will support cancer-related research over the next five years at The University of Texas at Dallas.
Two projects related to brain cancer, each totaling $200,000 over two years, recently received High-Impact/High-Risk Research Awards from the Cancer Prevention & Research Institute of Texas (CPRIT). A third CPRIT grant, of nearly $3.6 million over five years, will be used to establish a new core imaging facility for preclinical research. That award will be combined with $400,000 in matching funds from the University.
The Department of Defense (DOD) also recently awarded the University more than $527,000 for lung cancer research.
“UT Dallas research runs the gamut, from engineering and science to business and social issues,” said Dr. Joseph Pancrazio, vice president for research and professor of bioengineering. “But fundamental cancer research is one of the most important things we do, with the potential to impact so many lives. Ongoing support from CPRIT, the Department of Defense and other agencies ensures we can continue to make significant strides in improving human health.”
Brain Cancer Projects
Glioblastoma is a common and highly aggressive form of adult brain cancer. With treatment, the median survival is about 14.6 months after diagnosis, according to the American Brain Tumor Association.

Dr. Lloyd Lumata
Dr. Lloyd Lumata, assistant professor of physics, will use his $200,000 CPRIT grant to develop a new noninvasive imaging technique that could detect glioblastoma earlier and more accurately. The technique uses hyperpolarization technology to boost by more than 10,000-fold the sensitivity of MRI signals from key biological molecules associated with glioblastoma.
In addition to mapping cancer in the brain more precisely, the technology could reduce the need for patient exposure to X-rays from CT scans and radioactive imaging tracers, or for removal of brain tissue for diagnosis.
Dr. Zhenpeng Qin
Advancing from a previous CPRIT grant he received in 2016, Dr. Zhenpeng Qin, assistant professor of mechanical engineering, will use his new CPRIT funding for a project aimed at improving the delivery of drugs to brain tumors.
A major challenge to treating brain cancer is getting drugs across the blood-brain barrier, which is composed of densely packed cells that restrict and actively prevent the passage of substances from the bloodstream to the brain. Qin’s approach is to use nanoparticles that can be triggered with infrared light to perform molecular surgery on key proteins guarding the blood-brain barrier, thus allowing the delivery of anti-cancer drugs that were previously blocked by the barrier.
New Core Facility for Preclinical Studies

Dr. Kenneth Hoyt
Dr. Kenneth Hoyt, associate professor of bioengineering, is director of a new small-animal imaging core facility, established by a $3.6 million CPRIT grant.
The facility will include several powerful imaging instruments that will be used by cancer researchers to visualize and target tumors in small-animal models of the disease. Such studies allow researchers to test the efficacy of new diagnostic strategies and therapies prior to their use in humans.
Hoyt’s research is focused broadly on the development and use of novel ultrasound technologies for detecting, monitoring and treating diseases such as cancer.
His work has applications in targeted drug delivery and in personalized medicine, which maximizes the effectiveness of therapy for an individual patient.
New Approach to Lung Cancer Treatment
Dr. Jung-whan “Jay” Kim
In 2017 Dr. Jung-whan “Jay” Kim, assistant professor of biological sciences, published a study that showed one subtype of non-small cell lung cancer — squamous cell carcinoma — is more dependent on sugar to survive than other types of lung cancer.
With his Department of Defense grant, Kim will investigate whether this cancer’s addiction to sugar can be exploited as a potential new treatment strategy. He will test whether a very-low sugar diet as well as a widely used Type 2 diabetes drug can restrict sugar uptake and utilization to stop the growth of lung squamous cell carcinoma. Kim is also co-director of the small-animal imaging core, and he is a co-principal investigator on Lumata’s CPRIT grant.
Media Contact:
Amanda Siegfried, UT Dallas, 972-883-4335, amanda.siegfried@utdallas.edu, or the Office of Media Relations, UT Dallas, (972) 883-2155, newscenter@utdallas.edu.





