Chronic Pain Researchers Pursue New Path to Localized Relief
By: Stephen Fontenot | Feb. 25, 2022
Researchers from the Center for Advanced Pain Studies (CAPS) at The University of Texas at Dallas have teamed up with colleagues at the Marine Biological Laboratory (MBL), Yale School of Medicine and Tel Aviv University to pursue a new approach to localized chronic pain relief.
Their project received a $6.8 million grant from the National Institute of Neurological Disorders and Stroke, a component of the National Institutes of Health (NIH), for the first three years of a potential five-year project. The grant is part of the NIH’s Helping to End Addiction Long-term (HEAL) Initiative, which was created in response to the opioid epidemic. It funds efforts to develop nonaddictive analgesics and improve treatment for misuse of opiates.
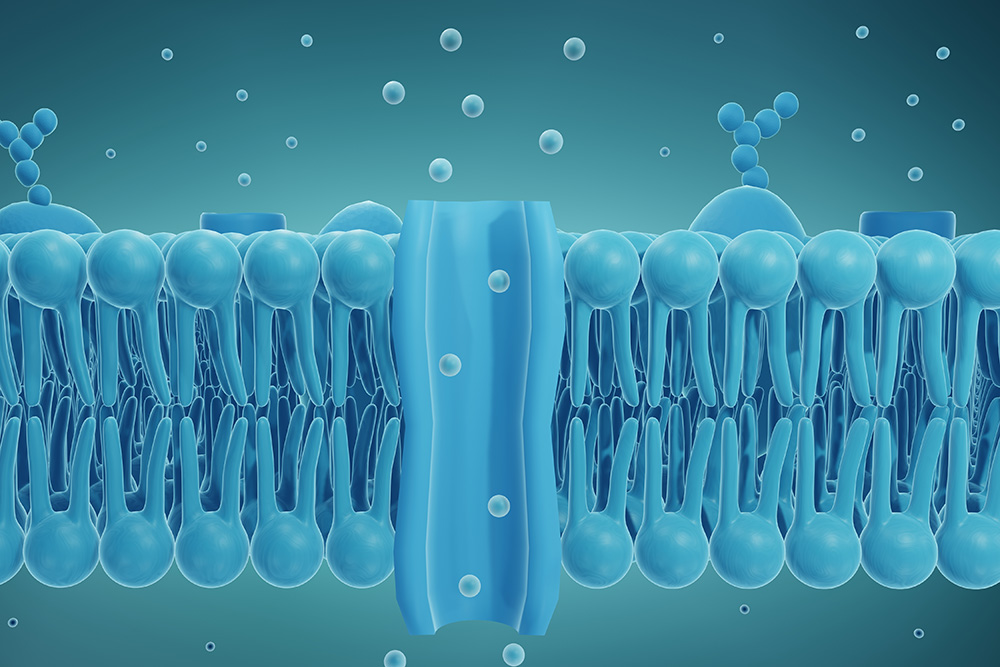
The research team is focusing on sodium channels, which are proteins in cell membranes that allow sodium ions into cells. That action creates electrical impulses in nerve and muscle tissue. Selectively blocking particular sodium channels to impede their signals can reduce neuron excitability and slow the signal rate down, potentially reducing pain at its molecular source.
The group’s target of interest is a sodium channel called Nav1.7.
“We don’t often get opportunities to work on a target like this that is so clearly validated in humans, where if you turn it off, you don’t feel pain, and if you turn it up, you feel too much pain,” said Dr. Gregory Dussor, a co-principal investigator on the project, Eugene McDermott Professor and chair of the neuroscience department in the School of Behavioral and Brain Sciences at UT Dallas.
“We’ve known about this channel for a long time. It’s particularly interesting in the context of pain,” Dussor said. “Studies over the past 10 to 15 years have shown that mutations in this channel can cause people to either have inability to sense pain or to suffer a chronic pain state.”
Altering RNA

Efforts to create a Nav1.7 blocker in pill form haven’t yet panned out. Dussor and his colleagues have another strategy in mind: altering the messenger RNA that carries the instructions to make the channel protein. They’re using a technique called site-directed RNA editing.
“This edit would change what is normally a sodium channel to a sodium and potassium channel,” Dussor said. “That has effects that minimize the ability of this protein to help generate electrical signals in neurons. To modify the RNA that’s making this channel protein would require an injection targeted at the pain site.”
Messenger RNA carries protein-making instructions that have been copied from a cell’s DNA. In RNA editing, these instructions are intercepted and modified on their way to the cell’s protein-making machinery. Because RNA is made only when needed and then degrades, the editing tactic has only a temporary effect, the duration of which is unclear.
“We don’t often get opportunities to work on a target like this that is so clearly validated in humans, where if you turn it off, you don’t feel pain, and if you turn it up, you feel too much pain.”
Dr. Gregory Dussor, Eugene McDermott Professor and chair of the neuroscience department in the School of Behavioral and Brain Sciences
“RNA is made when needed, and, when it degrades, the edits we will create will disappear, allowing the neuron to essentially go back to its prior state,” Dussor said. “If you give people maybe several months of pain relief using this approach, it’s possible that the nervous system could reset itself so the pain doesn’t come back.”
This model of treatment is not intended for acute, recent injuries, like fractures, Dussor said.
“This is more about years-long neuropathic pain for which other therapeutic approaches haven’t worked,” he said.
Team of Experts
Dr. Theodore Price BS’97, director of CAPS and Ashbel Smith Professor of neuroscience, said UT Dallas researchers joined the effort as the experts on preclinical modeling and therapeutic evaluation of various pain conditions, including postsurgical pain, neuropathic pain and migraine.
“This idea has been incubating for a long time. I think our first discussions were five years ago,” he said. “It is certainly great to be working with these collaborators from Yale and MBL.”
“It’s a really nice example of bringing together a collection of investigators with varied expertise and interests from different universities to try to get this to work,” Dussor said.
To learn more about how UT Dallas is enhancing lives through transformative research, explore New Dimensions: The Campaign for UT Dallas.
Dr. Joshua Rosenthal, MBL senior scientist and lead principal investigator (PI) on the project, has been developing the technology of RNA editing, primarily in invertebrates. His interest in sodium channels led him to collaborate with Yale School of Medicine’s Dr. Sulayman Dib-Hajj, senior research scientist in neurology, and Dr. Steve Waxman, professor of neurology and of neuroscience.
“Ted and I have known the Yale group for many years and have published with them previously,” Dussor said. “It’s great to now be working with the rest of the team.”
Dr. Eli Eisenberg, professor at Tel Aviv University, is also a co-PI on the project.
UT Dallas researchers will work on two of the project’s four sections. The preclinical modeling portion involves developing mice with a humanized version of the Nav1.7 channel. If their initial steps are successful, UT Dallas scientists will also contribute to the final section of the project, in which the RNA editing approach will be tested across various laboratory models of human pain and directly on sensory neurons isolated from humans.
“This is too big for a traditional grant. It could have been three separate grants, but the synergy of everything is part of the attraction of the project,” Dussor said. “Kudos to NIH for having the creativity to develop this platform as part of the HEAL Initiative. Without this kind of grant-funding mechanism, this large synergistic project doesn’t work.”
Media Contact:
Stephen Fontenot, UT Dallas, 972-883-4405, stephen.fontenot@utdallas.edu, or the Office of Media Relations, UT Dallas, (972) 883-2155, newscenter@utdallas.edu.





