A research assistant professor from The University of Texas at Dallas Center for Advanced Pain Studies (CAPS) has received a five-year, $3.1 million grant from the National Institutes of Health (NIH) to explore a potential biochemical trigger underlying diabetic neuropathy.
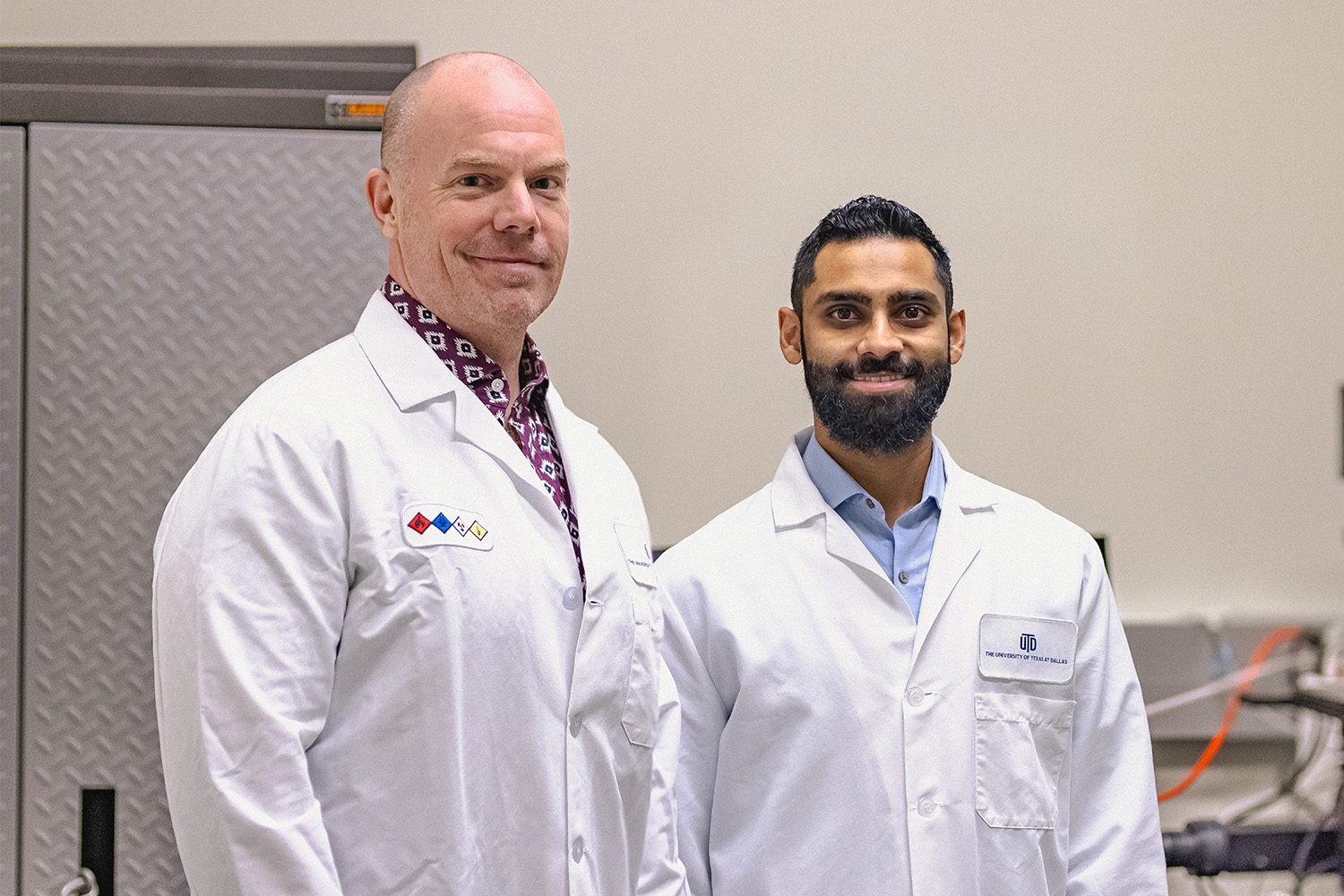
Dr. Muhammad Saad Yousuf in the School of Behavioral and Brain Sciences has teamed with scientists at Texas Tech University Health Sciences Center El Paso (TTUHSCEP) on the project. The researchers’ goal is to develop non-opioid therapies to relieve the chronic pain that reduces quality of life for about half of diabetic patients. More than 35 million Americans have diabetes.
“Diabetic neuropathy is different from most kinds of neuropathic pain because, in other cases, there is generally some kind of injury, like a damaged nerve,” Yousuf said. “Diabetic neuropathy is driven by a metabolic syndrome that’s circulating throughout the entire body, affecting more than just nerves.”
To learn more about how UT Dallas is enhancing lives through transformative research, explore New Dimensions: The Campaign for UT Dallas.
The study will address a subtype of diabetic neuropathy involving elevated levels of methylglyoxal, an organic compound that is a known biomarker for potential neuropathy. Yousuf and his collaborators suspect pain in diabetic patients is caused by methylglyoxal inducing the integrated stress response — a biochemical signaling pathway that helps cells adapt to changing conditions.
“Most biochemical events that stress a cell out — such as a lack of nutrients or viral infection — will initiate or promote the integrated stress response to try to reestablish balance,” Yousuf said. “But the response to an acute, brief stressor looks very different from a long-term stressor. Eventually, cells can no longer cope, and we believe the accumulated integrated stress response leads to nerve cells dying, causing neuropathic pain.”
One of the project’s aims is to determine how methylglyoxal makes human neurons hyperexcitable. The team will use donated human dorsal root ganglia cells to study the effects of the protein eukaryotic translation initiation factor 2α, or eIF2α.
“Dr. Yousuf’s new NIH project tackles the most common form of neuropathic pain — diabetic neuropathy — with a new viewpoint on how reactive metabolites known to cause pain in the disease act directly on sensory neurons to cause the underlying pathology,” said Dr. Ted Price BS’97, Ashbel Smith Professor of neuroscience and CAPS director. “His innovative use of nervous system samples recovered from organ donors with the Southwest Transplant Alliance will give direct translational insight into diabetic neuropathic pain.”
“If we learn what happens between methylglyoxal and the integrated stress response, and how the integrated stress response alters neuronal behavior, we can test drugs that inhibit the integrated stress response.”
Dr. Muhammad Saad Yousuf
The integrated stress response starts with the phosphorylation and inhibition of eIF2α and the activation of an alternative protein, eIF2A. Although their names are similar, eIF2α and eIF2A have differing effects on the production of proteins that are ultimately responsible for pain. This project seeks to uncover which proteins are important for pain caused by methylglyoxal. Using both human cells and knockout mice — in which the EIF2A gene is intentionally “knocked out,” or deactivated — researchers will investigate how that gene affects the integrated stress response.
“Knockout animals allow us to understand a pathway and try to pinpoint a characteristic or behavior that we can go back and correct,” Yousuf said. “Initial experiments show that losing eIF2A protects against evoked and spontaneous pain caused by methylglyoxal injections.”
He said access to human dorsal root ganglia cells — a rare resource in the scientific community — allows the team to validate animal model conclusions in human cells before proceeding to clinical trials in human subjects.
“If we learn what happens between methylglyoxal and the integrated stress response, and how the integrated stress response alters neuronal behavior, we can test drugs that inhibit the integrated stress response,” Yousuf said. “While it would be a new approach to pain treatment, such drugs are already in clinical trials to treat ALS [amyotrophic lateral sclerosis, or Lou Gehrig’s disease] and Alzheimer’s disease, and so far, it appears that certain approaches are generally safe.”
The research is funded through the NIH’s National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Munmun Chattopadhyay, associate professor in the Center of Emphasis in Diabetes and Metabolism at TTUHSCEP, is a co-principal investigator on the project.
Study: Researchers Pinpoint Target for Neuropathic Pain Relief
University of Texas at Dallas researchers from the Center for Advanced Pain Studies (CAPS) teamed with colleagues from UT Austin and the University of Miami Miller School of Medicine to publish findings about a molecule that, when it binds to a cell membrane protein called sigma-2 receptor, alleviates neuropathic pain and inhibits the integrated stress response.
Dr. Ted Price BS’97, Ashbel Smith Professor of neuroscience and CAPS director, is co-corresponding author of the paper published Dec. 20, 2023, in the Proceedings of the National Academy of Sciences, along with UT Austin chemistry professor Dr. Stephen F. Martin. UT Dallas research assistant professor Dr. Muhammad Saad Yousuf is the lead author.
In the study, the researchers described a new sigma-2 receptor binding compound called FEM-1689, which was designed by UT Austin scientists. They introduced the compound in a rodent model, where it targeted those receptors and reduced pain hypersensitivity and the integrated stress response without involving opioid receptors. The scientists then tested the compound on isolated human sensory neurons, showing similar effects that suggest sigma-2 receptors are promising targets in the treatment of neuropathic pain.
“This work is the culmination of a wonderful five-year collaboration with our colleagues at UT Austin and is a great example of academic drug discovery pushing the field of non-opioid pain therapeutics forward,” Price said. “Our funding from NIH on this continuing project through our spin-out company, NuvoNuro, has the potential to take us toward clinical development in the next few years, which is extraordinarily exciting.”
Martin, Price and Yousuf are among the co-founders of NuvoNuro.

