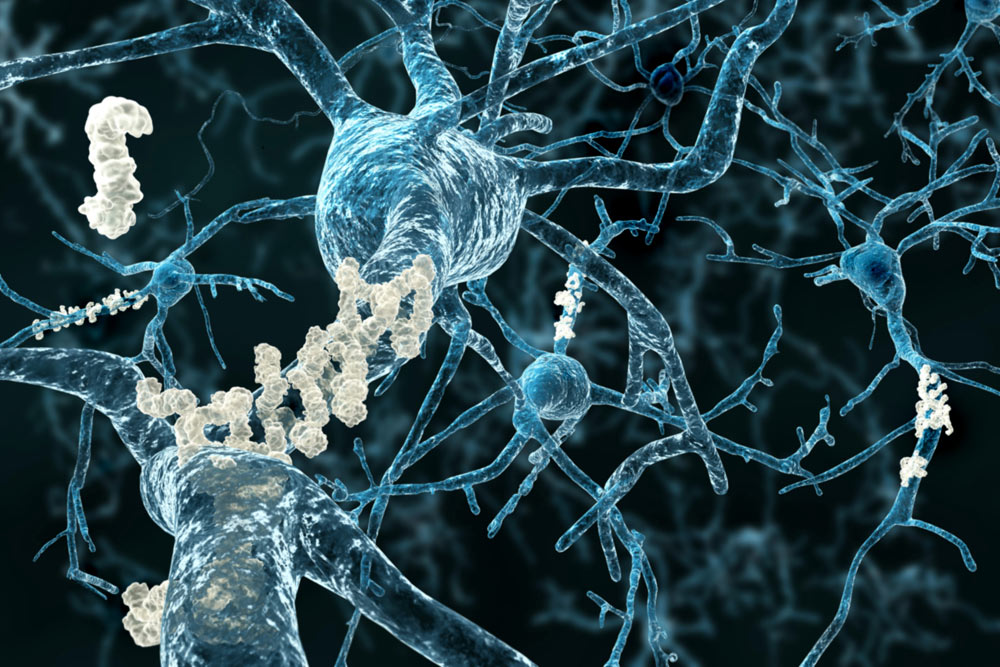
In recent years, neurology researchers have shown that accumulation of the protein beta-amyloid in the brain is strongly linked to the occurrence of Alzheimer’s disease (AD). Excessive amounts of beta-amyloid alone, however, rarely seem to cause Alzheimer’s without other contributing factors.
Scientists from The University of Texas at Dallas’ School of Behavioral and Brain Sciences hope to understand better the relationship between beta-amyloid and iron accumulation and their roles in the degradation of memory. Their latest study, published in the Nov. 3, 2020, print issue of Neurology, suggests that iron and beta-amyloid may both contribute to shrinkage of the entorhinal cortex, a region of the medial temporal lobe of the brain essential for the processing and recording of memories.
“We hope to find better, earlier ways of determining that someone is on a pathway to developing Alzheimer’s disease, enabling potential treatments to start sooner,” said senior author Dr. Karen Rodrigue, associate professor of psychology and director of the Cognitive Neuroscience of Aging Lab in the Center for Vital Longevity (CVL). “At the same time, we also advance understanding of the basic mechanisms of how the brain works and ages.”
AD is the sixth-leading cause of death in the U.S. and affects more than 5.5 million Americans. The disease is believed to result from a chain of processes in the body that must occur in a specific order.
“This research provides evidence that, in cognitively normal adults, increased iron content and beta-amyloid plaque coincide with reduced entorhinal cortex volume,” Rodrigue said.

“In this initial study, while we did not demonstrate a direct relationship between iron and beta-amyloid accumulation, we do find that people who had more of both showed smaller volumes in the entorhinal cortex. Beta-amyloid alone did not reveal these associations — only the joint effect of iron and beta-amyloid.”
Dr. Karen Rodrigue, associate professor of psychology and director of the Cognitive Neuroscience of Aging Lab in the Center for Vital Longevity
The study, funded in part by the National Institutes of Health (NIH), involved 70 neurologically healthy participants with a mean age of 68 who underwent cognitive testing, as well as positron emission tomography and MRI scanning at UT Southwestern Medical Center.
“In this initial study, while we did not demonstrate a direct relationship between iron and beta-amyloid accumulation, we do find that people who had more of both showed smaller volumes in the entorhinal cortex,” she said. “Beta-amyloid alone did not reveal these associations — only the joint effect of iron and beta-amyloid. So, it’s among the first evidence that iron may play an important contributory role to the early changes that precipitate AD.”
‘Crosstalk’ Focus
In the past 15 years, scientists have developed methods to examine beta-amyloid levels in the brains of living humans. Indications are that beta-amyloid dysregulation happens early — long before symptoms appear.
“While we mostly study healthy aging in my lab, a portion of those people may already be on a path to Alzheimer’s and not know it,” Rodrigue said. “It has become clear that an important component of understanding and preventing AD lies in studying healthy aging.”
Dr. Chris Foster, a postdoctoral scientist in Rodrigue’s lab and the lead author of the paper, explained that the entorhinal cortex’s importance for memory is well established.

“The hippocampus is where memory is ultimately encoded, but it requires input — something to take all the sensory data and funnel it to become memories,” he said. “That seems to be the role of the entorhinal cortex. AD is thought of as a memory disorder, primarily because early in the disease process it attacks regions of the brain — such as the entorhinal cortex — that provide key input into the hippocampus.”
Although iron and beta-amyloid have each been widely studied for their respective roles in Alzheimer’s, Foster said few researchers are examining the “crosstalk.”
“This is some of the first work that gives us a hint that these pathways interact in a meaningful way,” he said.
While beta-amyloid is most commonly known for its negative effects when present in large amounts, Foster emphasized that both it and iron are essential for neurological function.
“Like with other parts of the body, many things are necessary in a certain amount for our brains to function,” he said. “If you put those out of regulation, they become a problem. Beta-amyloid and iron both help the brain function, but when dysregulated, they cause oxidative stress, which is thought to damage neurons and supporting tissue.”
Foster highlighted the importance of not viewing an individual potential culprit in isolation when so many interactions are occurring.
“We often find ourselves in a silo as researchers, focused on a single thing. That leaves us susceptible to overlooking interactions that can be crucial,” he said. “We are helping build a better understanding of cross-modal interactions that lead to negative outcomes — ones that are not well explained by any single-path model.”
What’s Next
With participant data available from a single point in time, researchers hope to replicate the results in the near future with the same group of subjects to create a longitudinal picture of changing beta-amyloid and iron levels, as well as entorhinal cortex size.
“When these people come back to the lab, will we see further entorhinal shrinkage, and is that shrinkage still correlated to the beta-amyloid and iron in the same way?” Rodrigue said.
At the Speed of Bright
UT Dallas has earned a reputation for incredibly bright students, innovative programs, renowned faculty, dedicated staff, engaged alumni and research that matters. Read stories about more of the University’s bright stars.
Foster hypothesizes that “cognitively normal people with high amyloid and iron levels who are showing age-based effects on entorhinal cortex volume are likely to be more susceptible to memory decline. But the longitudinal study necessary to test that question is still underway.”
Rodrigue said that these findings go beyond studying one disease, however important that condition may be.
“The applications of this type of work are not only for preclinical stages of AD, but also about healthy aging,” she said. “There’s a remarkable amount of neurological variance in healthy aging. Maybe we learn some nuance about beta-amyloid in the future that tells us this isn’t simply a story about AD. And maybe we’ll have results that help us better understand and predict the variability in cognitive decline within healthy aging.”
Other authors of the paper were Dr. Kristen Kennedy, associate professor of psychology and director of the Neuroimaging of Aging and Cognition Lab in the CVL; and Dr. Ana Daugherty, director of the Healthy Brain Aging Laboratory at Wayne State University.
The work was funded by three grants — 5R00AG036848, 5R00AG036818 and 5R01AG057537 — from the National Institute on Aging, a branch of the NIH; and by the Alzheimer’s Association, Eli Lilly and Co., BvB Dallas and AWARE.